The strategy you will need to survive a Parkinson's disease hospitalization
Drs Ariane Carpentier, Ramzi Salloum and I recently wrote an editorial on the ‘sources of harm’ for Parkinson’s disease (PD) persons and we presented potential solutions for the healthcare system (2023). Our editorial comment was based on the recent article by Ritzi and Walter from the Cleveland Clinic Foundation (2023 Parkinsonism and Related Disorders).
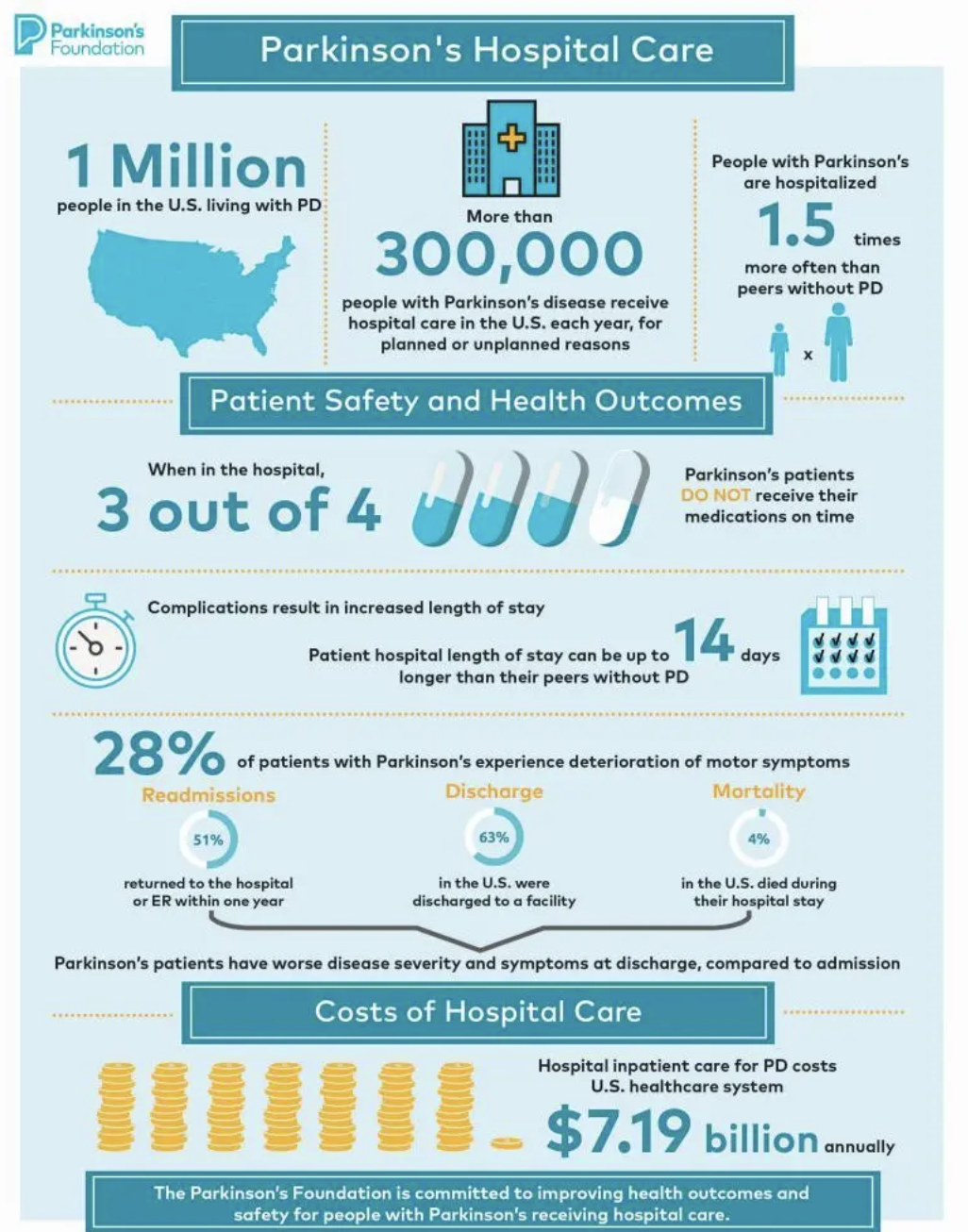
The hospital is a dangerous destination for persons with PD. Achieving the highest quality inpatient hospital care for persons with PD is not as ‘straight-forward’ as you may think. Each year, approximately one third of persons with PD will visit the emergency department or will be admitted to a hospital.
Do you know the common reasons why folks with PD end up in the hospital? Do you know what are the common ‘timing’ and ‘type’ of medication issues which may impact a hospitalization. What is on your checklist and are you ready with a plan if you end up in the hospital?
What is the bottom line: The numbers of persons with PD who will present to the hospital is alarming, the preventable mistakes are striking and the cost to the health care system is staggering.
Is the hospitalization rate with Parkinson’s disease higher compared to those without Parkinson’s?
This paper using Parkinson’s Foundation data showed that hospitalization rates were higher. The paper also showed re-admission rates were also higher (Shangholi, 2017).
Hospitalization rates in PD are higher, admissions are more prolonged and not surprisingly, persons with PD experience more complications when hospitalized. Not only is the hospitalization rate higher but the re-hospitalization rate is also higher.
In the Parkinson’s Outcome Project sponsored by the Parkinson’s Foundation, 7,507 persons with PD the significant factors associated with a history of a hospital encounter included race (white race: OR 0.49), utilization of physical therapy (OR 1.47), history of deep brain stimulation (OR 1.87), number of co-morbidities (OR 1.30), caregiver strain (OR 1.17 per standard deviation), and the standardized Timed Up and Go Test (OR 1.21). A history of hospitalization was associated with re-hospitalization (HR1.67, P<0.0001) (Hassan, Parkinsonism and Related Disorders, 2013), (Shangholi, PLOS ONE, 2017).
What are the common reasons persons with Parkinson’s seek a hospital?
Annette Schrag and colleagues in 2020 reviewed the published literature on hospitalization in Parkinson’s disease (Parkinsonism and Related Disorders).
What were the leading causes of hospitalization in Parkinson’s disease?
Infections in 22% (mainly urinary tract infections and pneumonia)
Worsening of motor symptoms in 19%
Falls and fractures in 18%
Cardiovascular (heart and blood vessel) related issues in 13%
Neuropsychiatric (for example behavioral issues such as depression, anxiety, hallucinations) occurred in 8%
Gastrointestinal (gut) symptoms in 7%
Will the numbers of persons with Parkinson in the hospital increase or decrease in the future?
New data is out on Parkinson’s disease and it suggests that previously we ‘underestimated’ how much Parkinson’s disease is really ‘out there (Willis, Nature Parkinson Disease, 2022).’ A new case of PD is diagnosed every 6 minutes (compared to every 9 minutes on previous estimates). As the population of persons with PD continues to rise (globally), the number of persons with Parkinson’s in the hospital setting will not surprisingly grow.
To reduce morbidity and mortality of Parkinson’s hospitalization, proactive strategies are critically needed to address the barriers in implementing ‘practical and preventative’ measures among hospitalized persons.
Why is the hospital a dangerous place if you have Parkinson’s disease?
Daniel Martinez showed in 2015 that administration of neuroleptics was associated with a longer hospital stay in Parkinson’s (Martinez, PLOS ONE, 2015).
It turns out, there are many factors which contribute to the dangers a person with PD may encounter during hospitalization. Jeryl Ritzi and Ben Walter at the Cleveland Clinic recently published a study aimed at ‘establishing a framework for the quality of inpatient care for PD’ and their work highlighted one of the most important factors: the complexity of PD medication administration. Their study showed there were important deviations between outpatient and inpatient medication administrations and that many of these errors could be preventable.
The authors revealed that there were three important observations which were driving medication administration errors:
1- Errors in medication dosage (total levodopa equivalent dose (LEDD).
2- Deviations in medication timing
3- The inappropriate use of dopamine blocking medications.
Here were some surprising findings:
Levodopa formulation substitutions and deviations from levodopa equivalent dosages occurred in 19% of inpatient hospitalization days.
There were possible changes in formulation because the physician or advanced practice provider restricted the prescription of oral (by mouth) formulations of medications. Could a nasogastric tube be used?
There were changes due to medication ‘unavailability,’ and these frequently led to deviations in the doses of medications.
What can you do if a hospital does not have your particular Parkinson medication on their formulary?
The availability of individual medications in a hospital will differ from facility to facility and region to region.
We suggest allowing persons with PD to provide a supply of their home medications at the time of admission. Usually a doctor or an advanced practice provider can write this order.
In cases where a medication substitution is unavoidable use the most updated conversion formulas.
Are medications delivered ‘on time’ in the hospital for persons with Parkinson’s disease?
Studies from the Parkinson’s Foundation have shown that 3/4 persons with PD do not receive their medications on time every time. Ritzi and Walter in their study, similarly showed that about half of medication administrations deviated by at least 30 minutes when compared to the timing of the outpatient clinic medication schedule. Collective evidence in PD suggests that even slight variations in medication timing can increase the risk of motor fluctuations, dysphagia, and falls. Also, medication errors have been directly associated with worsening in motor function.
In Ritzi and Walter’s recent paper, the authors reported many concerning challenges especially with receiving levodopa on time and receiving it at the appropriate dosage (compared to outpatient medications).
Ritzi and Walter’s recent 2023 paper in Parkinsonism and Related Disorders showed many concerning issues with folks receiving the wrong levodopa dosage and in many cases not receiving PD medications ‘on time.’
Does medication ‘timing and type’ contribute to longer hospital stays in Parkinson’s disease?
As an excellent example of a local/regional network improving quality, ‘Coffs Clinical Network’ implemented a clinical guideline procedure to improve the delivery of safe and timely medications to people with PD.
Ritzi and Walter, like Martinez (2015) and similar to other studies showed that deviations in medication timing were associated with a longer length of stay.
It turn’s out the two T‘s are critical to safety in the hospital setting for any person with PD.
Timing of medications is critical and orders should be written or typed with ‘specific times’ associated with each administration.
The second ‘T’ is the type of medication. Most dopamine blockers are ‘bad’ and can contribute to morbidity and potentially mortality in the PD hospital setting. The three safest dopamine blockers in PD are clozapine, quetiapine and pimavanserin.
How often do hospitalized persons with Parkinson’s receive dopamine blocking medications?
In the Ritzi study, dopamine blocking medications capable of worsening PD were prescribed in an alarming 10% of admissions. In these cases, haloperidol was administered in 35% , followed by olanzapine in 23% and metoclopramide in 17%. Administering these medications was associated with a longer length of stay, an increase in mortality and an increase in re-admissions.
Remember, the three best anti-psychotic medications for PD (clozapine, quetiapine and pimavanserin) are ‘safer’ than the other dopamine blockers for PD, however since they are all pills, a nasogastric or feeding tube may be required for administration (in select cases).
What are practical and proactive Parkinson’s hospitalization measures which may lead to better outcomes?
Carpentier and colleagues outlined three areas where we can improve and potentially prevent errors during Parkinson’s disease hospitalizations (Carpentier, Parkinsonism and Related Disorders, 2023).
1. Adherence to Outpatient Medication Regimens
· Adhere to current outpatient medication regimens when persons with PD are hospitalized, except in cases of acute PD medication-related issues.
· Confirm the PD medication list with the person with PD and their caregiver.
· Document specific timing of orders in the electronic health record (e.g., carbidopa levodopa 25/100 1 pill at 8am, 1 pill at 12pm, 1 pill at 4pm and 1 pill at 8pm).
· Write an order allowing the use of at-home medications especially when not available on the hospital formulary. Persons with PD and their care partners who are capable of administering medications with precise timing should be granted this privilege.
· Consider an early consultation with an inpatient neurologist coincident with or soon after admission.
2. Education and Training for Healthcare Providers
· Provide comprehensive education and training for all hospital-based healthcare providers who may care for a person with PD. Education should include medications and potential future PD hospitalization.
· Educate providers on strategies to facilitate frequent and timely administration of medications to minimize the errors in doses and in timing of PD medications.
· Educate providers on the acute management of persons with PD who cannot take oral medications.
· Educate providers on the management of PD related devices (e.g., deep brain stimulation implants, pumps).
· Educate providers on imaging guidelines for individuals with PD who have deep brain stimulation implants.
· Educate providers on the benefits of rehabilitation therapies for PD in the inpatient setting (physical therapy (PT), occupational therapy (OT), speech and swallow therapy), especially for mobility, fall prevention and for reducing aspiration risk.
3. Implementation of Electronic Health Record Tools
· Implement alerts specifically designed for individuals with PD who are hospitalized.
· Use alerts to flag potentially contraindicated dopamine blocking medications.
· Use alerts to reinforce the precise timing of medication administration.
Do you have a proactive plan for Parkinson’s disease hospitalization?
What is the bottom line for Parkinson’s disease hospitalization? Over the course of your disease you can ‘count on a hospitalization and re-hospitalization’ happening at some point. You need a practical proactive and preventative plan to survive and to hopefully transform the hospital experience into a successful one.
The best plan is to: ‘have a plan’ and to proactively be prepared for the day when it arrives. One easy way to be prepared for Parkinson’s hospitalization is to obtain or to download the Parkinson’s Foundation Aware in Care kit. Follow the directions for each of the components of the kit, and most important don’t forget to take it with you to the hospital.
Avoiding a hospitalization by utilizing regular medical care with your general doctor and neurologist and by accessing outpatient services early may ‘save a hospitalization.’
Early identification and intervention for urinary tract and other infections.
Continuous monitoring in the outpatient setting for fall risk coupled with continuous attention to updating strategies to prevent falling.
Continuous monitoring and early intervention in the outpatient setting for hallucinations, psychosis, depression, anxiety or other behavioral changes.
Michael Okun along with Indu Subramanian are the blog co-editors and provide the content for the parkinsonsecrets.com blog.
Jonny Acheson is a person with Parkinson’s and the artist for parkinsonsecrets.com
Selected References:
*There are many authors over the previous decades who have contributed meaningfully to our understanding of Parkinson’s disease hospitalization. Below is a brief list of the work cited for this blog. We acknowledge the amazing work by ALL clinicians, scientists and persons with PD who have contributed to this critical body of research on PD hospitalization.
Okunoye O, Kojima G, Marston L, Walters K, Schrag A. Factors associated with hospitalisation among people with Parkinson's disease - A systematic review and meta-analysis. Parkinsonism Relat Disord. 2020 Feb;71:66-72. doi: 10.1016/j.parkreldis.2020.02.018. Epub 2020 Feb 28. PMID: 32156461.Establishing a framework for quality of inpatient care for Parkinson's disease: A study on inpatient medication administration
Jeryl Ritzi T. Yu, Claire Sonneborn, Olivia Hogue, Debolina Ghosh, Anne Brooks, James Liao, Hubert H. Fernandez, Shannon Shaffer, Scott A. Sperling, Benjamin L. Walter Establishing a framework for quality of inpatient care for Parkinson's disease: A study on inpatient medication administration. Published:July 07, 2023DOI: https://doi.org/10.1016/j.parkreldis.2023.105491
Shahgholi L, De Jesus S, Wu SS, Pei Q, Hassan A, Armstrong MJ, Martinez-Ramirez D, Schmidt P, Okun MS. Hospitalization and rehospitalization in Parkinson disease patients: Data from the National Parkinson Foundation Centers of Excellence. PLoS One. 2017 Jul 6;12(7):e0180425. doi: 10.1371/journal.pone.0180425. PMID: 28683150; PMCID: PMC5500337.
Zeldenrust F, Lidstone S, Wu S, Okun MS, Cubillos F, Beck J, Davis T, Lyons K, Nelson E, Rafferty M, Schmidt P, Dai Y, Marras C. Variations in hospitalization rates across Parkinson's Foundation Centers of Excellence. Parkinsonism Relat Disord. 2020 Dec;81:123-128. doi: 10.1016/j.parkreldis.2020.09.006. Epub 2020 Oct 3. PMID: 33120073.
Aminoff MJ, Christine CW, Friedman JH, Chou KL, Lyons KE, Pahwa R, Bloem BR, Parashos SA, Price CC, Malaty IA, Iansek R, Bodis-Wollner I, Suchowersky O, Oertel WH, Zamudio J, Oberdorf J, Schmidt P, Okun MS; National Parkinson Foundation Working Group on Hospitalization in Parkinson's Disease. Management of the hospitalized patient with Parkinson's disease: current state of the field and need for guidelines. Parkinsonism Relat Disord. 2011 Mar;17(3):139-45. doi: 10.1016/j.parkreldis.2010.11.009. Epub 2010 Dec 14. PMID: 21159538; PMCID: PMC3070297.
Hassan A, Wu SS, Schmidt P, Dai Y, Simuni T, Giladi N, Bloem BR, Malaty IA, Okun MS; NPF-QII Investigators. High rates and the risk factors for emergency room visits and hospitalization in Parkinson's disease. Parkinsonism Relat Disord. 2013 Nov;19(11):949-54. doi: 10.1016/j.parkreldis.2013.06.006. Epub 2013 Jul 5. PMID: 23835430.
Chou KL, Zamudio J, Schmidt P, Price CC, Parashos SA, Bloem BR, Lyons KE, Christine CW, Pahwa R, Bodis-Wollner I, Oertel WH, Suchowersky O, Aminoff MJ, Malaty IA, Friedman JH, Okun MS. Hospitalization in Parkinson disease: a survey of National Parkinson Foundation Centers. Parkinsonism Relat Disord. 2011 Jul;17(6):440-5. doi: 10.1016/j.parkreldis.2011.03.002. Epub 2011 Apr 1. PMID: 21458353; PMCID: PMC3895941.
Veilleux Carpentier A, Salloum RG, Okun MS. Practical proactive and preventative Parkinson's disease strategies for management in the hospital setting. Parkinsonism Relat Disord. 2023 Jul 4:105515. doi: 10.1016/j.parkreldis.2023.105515. Epub ahead of print. PMID: 37453869.